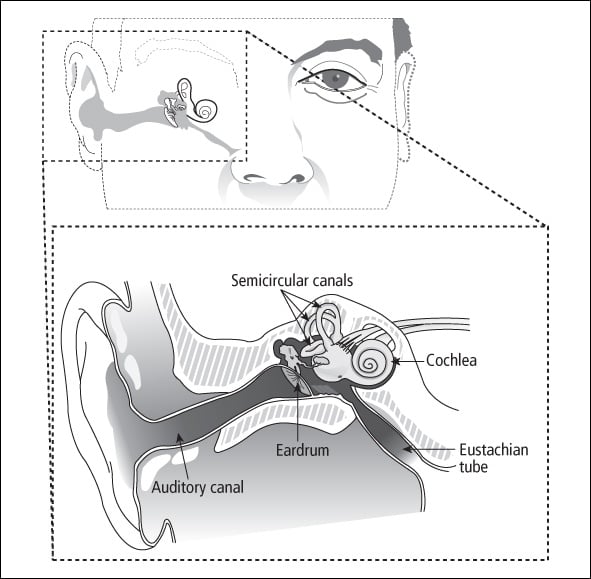
The ear, the organ of hearing, is made up of three main parts: external, middle, and inner ear. The external ear includes the outer portion (auricle) and the external auditory canal. The middle ear is a cavity separated from the external ear by the eardrum, and it contains three small bones. The inner ear contains the cochlea (which is responsible for hearing), the vestibule (which senses position in space and motion), and the semicircular canals (which control equilibrium). Figure 10-2 shows the anatomy of the ear.
Organ damage
Ears and hearing can be damaged by chemotherapy, high-dose radiation, and some antibiotics.
Chemotherapy
Some anticancer drugs, primarily cisplatin, can cause substantial hearing loss in the high- to ultra-high-frequency range—6,000 to 12,000 Hertz (Hz). If more damage occurs, the lower frequencies also can be affected. Carboplatin is also associated with hearing loss but to a much lesser degree. Radiation to the head can intensify the hearing loss from cisplatin.
My daughter Sarah had an ependymoma treated with radiation when she was 4 and chemotherapy when it returned at age 6. She had a baseline audiology test before the chemotherapy and then another after the second chemotherapy. Because of the change in her hearing, the cisplatin was removed from the remaining two cycles of chemotherapy called for in her protocol. The doctors think that some of the chemotherapy side effects—including the hearing loss—were a result of the chemotherapy compounding damage already done by the radiation. She has high-frequency loss and her low frequencies are at the low end of “normal.”
The damage generally occurs in both ears and is irreversible. Sometimes ringing in the ears (tinnitus) or a sensation of drifting in space or having objects drift around you (vertigo) can also occur. Children most at risk for chemotherapy-caused hearing loss are those treated for brain tumors, germ cell tumors, osteosarcoma, and neuroblastoma.
My daughter has mild-to-moderate high-frequency hearing loss after treatment for osteosarcoma. The hearing tests were, she says, the very worst part of cancer treatment because she knew she should be able to hear certain sounds and couldn’t. Now, as a college freshman 6 years off treatment, she just got hearing aids. Adjusting to them is difficult, but she wants them and will persevere. She also has constant tinnitus, but she has adjusted to it.
Radiation
Survivors who had head and neck tumors treated with higher doses of radiation and/or older radiation techniques (from the 1950s and 1960s) often develop hearing loss. The most common diseases treated with high-dose radiation that can affect the ears are as follows:
-
Nasopharyngeal carcinomas
-
Parameningeal sarcomas
-
Brain stem gliomas
-
Medulloblastomas
-
Ependymomas
Ethan’s treatment for medulloblastoma, which included cisplatin, caused high-end hearing loss, which means that in rooms with a lot of people he can’t hear at all. So at parties, he would kind of zone out because he really couldn’t hear what people were saying to him, but in the classroom he was okay. But then he started to have hearing loss that was related to the radiation, and he lost hearing in the voice recognition range. He was only catching about 60–70% of what people were saying. Because of the kind of hearing loss it was, hearing aids were only of limited use, and because he was still growing, they had huge molds that really irritated him. So he didn’t wear them.
The good news is that he’s learned to lip read. The bad news is that as a 17-year-old high school student he is less adept at letting people know he needs to lip read, so he still misses big chunks of conversation. Ethan is very compliant with all the things that he needs to do related to learning—he sits in the front of the room, he has someone who reads tests to him because he can’t read well enough, and all sorts of things that make him “different.” But the hearing loss is something he doesn’t really get yet. I know adults that had hearing loss as children who assure me that at some point this light bulb will go off for him and he will want to do what he can to compensate for it.
Children treated with less than 2400 cGy of cranial radiation (e.g., for leukemia or prior to stem cell transplantation) rarely develop any late effects in the ears.
Outer ear infections, which are common after high-dose radiation, can impair hearing by drying out and thickening the external ear canal and eardrum. Chronic middle ear infections (otitis media) can also be caused by radiation due to damage to the eustachian tube, which is responsible for drainage of the middle ear. When the eustachian tube cannot drain properly, middle ear infections can become chronic.
One effect that we were not warned of in advance has been a major problem. Joseph’s sinuses, and particularly his eustachian tubes, were damaged enough by the 5000 cGy of radiation to the orbit that he has a real problem with sinus infections and ear infections. The sinus infections were worse during the year of chemotherapy but are still an ongoing problem 2 years later. The ear infections are definitely getting worse as the damage to the tubes is apparently making itself known, in conjunction with his existing allergies. His hearing has been so reduced by the fluid buildup lately that he’s on Claritin ® , and his pediatrician and the ENT (ear, nose, and throat specialist) are talking ear tube surgery.
The glands that produce earwax (cerumen glands) may produce less wax, and what is produced sometimes gets crusty and impacted. While the earwax is impacted, hearing is decreased and trapped moisture can increase the risk for ear infections. This late effect can also occur in survivors who developed graft-versus-host disease after stem cell transplantation. Impacted earwax can be removed by your healthcare provider. Using cotton-tipped applicators or other objects in the ear canal is strongly discouraged because they can actually push impacted earwax further into the ear canal.
Clare was tested post-treatment and she just had a very minor loss in the high-frequency range, probably from gentamicin (an intravenous antibiotic). However, she has had a different type of hearing loss the last few months, in the low-frequency range and more extensive. We have been to the follow-up clinic several times and they decided it was the huge earwax build-up as a result of the radiation.
An extremely unusual late effect of radiation to the ear is inflammation of the cartilage (chondritis), which can lead to cartilage damage and infection. This can occur after radiation doses of more than 7800 cGy given for brain stem gliomas.
The risk factors for permanent hearing loss in children or teens treated for cancer are as follows:
-
Treatment with cisplatin, and to a lesser extent, carboplatin
-
High doses of radiation to the head and/or neck
-
Younger age at time of treatment
-
Surgery involving the ear, brain, or auditory nerve
-
Treatment with certain antibiotics such as gentamicin and amikacin (generally used for serious infections or fever when blood counts are low)
-
Chronic ear infection
-
Treatment with diuretics (drugs that help the body get rid of excess water)
-
Poor kidney function
Signs and symptoms
Hearing loss should be suspected if your child:
-
Does not startle or respond to loud noises.
-
Does not respond to your voice consistently.
-
Has a hard time understanding or following directions after age 3.
-
Does not have clear speech.
-
Fails to develop sounds or words that are appropriate for her age.
-
Uses gestures instead of words.
Signs and symptoms of hearing loss typically associated with chemotherapy may be less obvious but should be suspected if your child:
-
Confuses like-sounding words.
-
Drops sounds off words or reports not hearing sounds such as th, f, sh, s, t, k, g, ch, and v.
-
Reports he can hear but not understand words and speech.
-
Has difficulty hearing in noisy situations or environments.
School-aged children who have lost some hearing may withdraw socially or have trouble in school. They may also describe ringing in their ears or dizziness.
My daughter Erin, who was treated for osteosarcoma, lost a fair amount of her hearing due to cisplatin. She doesn’t think it’s bad enough for hearing aids although they probably would help her a bit. She said when she went to the Young Adults Conference at Camp Mak-A-Dream, everyone who had trouble hearing would tap their ears and say “Cisplatin” as a reminder to speak up!
Screening and detection
After treatment ends, appointments at the follow-up clinic should include an ear examination to look for infection, wax buildup, and eardrum perforation or scarring. Survivors should also have their hearing tested periodically following completion of treatment, because chemotherapy can have an impact on hearing up to 5 years after completion of the last round. Healthcare providers of survivors who had head or brain radiation may recommend periodic hearing tests because hearing problems can also sometimes develop several years after radiation. Anyone with abnormal test results should be referred to an audiologist or otolaryngologist (ear, nose, and throat doctor) for a thorough evaluation to determination whether assistive technology would be helpful.
I had cisplatin to treat my osteosarcoma. I lost some of my high-frequency hearing, but not enough to get hearing aids. It’s worse in one ear than the other, because when I’m lying on one side I can hear my college roommate if she’s talking, but I can’t if I’m lying on the other side. I still get ringing in my ears that lasts for a few seconds then goes away.
The most widely used method to test the hearing of children with cancer is pure tone audiometry. These tests should be administered by an experienced pediatric audiologist. Extended high-frequency audiometry may be used to test for hearing loss in the high-frequency range (4,000 to 20,000 Hz). This is especially important for younger children with limited language because many consonants (“th”, “f”, “p”, “s”) are in this range. If a child cannot hear these consonants it may be very hard for her to acquire clear speech, so early intervention can make an important difference.
Degrees of hearing loss, measured in decibels (dB), are:
-
Mild (25–40 dB): Difficulty hearing distant speech, soft voices, or voices in a noisy place.
-
Moderate (45–60 dB): Difficulty hearing speech in a quiet place.
-
Severe (65–90 dB): Cannot hear loud voices or sounds.
-
Profound (more than 90 dB): May hear only very loud sounds, and must rely more on vision than hearing to understand communication if they are not wearing hearing aids or have a cochlear implant.
Children at risk for hearing loss should also be tested for speech and language disorders. Assessments such as the Rossetti Infant Toddler Language Scale (used with children from birth to 36 months), the Preschool Language Scale 5th edition (used on children from birth to age 7), and the Goldman-Fristoe Test of Articulation 2nd edition (used on children ages 2 to 21) are used to identify speech and language disorders and evaluate the effectiveness of hearing aids, auditory training, and speech therapy programs.
Medical management
Medical management includes treating middle or external ear infections, and in some cases, placing tubes in the ears. Survivors with tinnitus (ringing in the ears) may benefit from intervention and should be evaluated by an audiologist or otolaryngologist. State-of-the-art hearing aids are needed for those with permanent hearing impairment. Newer digital technology can minimize background noise and maximize speech sounds, unlike hearing aids of the past. Proper fitting and follow-up testing are crucial. It is also important to develop a routine for maintaining the aids, cleaning the ear molds, and replacing the batteries. Ear molds will need to be replaced periodically; an indication that they should be checked is “feedback” or high-pitched noise coming from the hearing aids. Fostering language development with speech reading and signing is vital for those with profound hearing loss. Using the closed captioning while watching television can also be helpful. Coping with the emotional and psychological effects of hearing loss in children and teens is an essential component of care.
Sarah wears hearing aids now and it hasn’t been a problem. I give full credit to my husband. In the week before she got them, he regularly told her that there was a way to make her hearing better and wouldn’t that be great. Sarah’s hearing literally went overnight and the hearing aids brought her hearing back overnight, so she knows what a difference they make. The technician at the hearing clinic let her pick the color of the ear molds. She picked bright pink. Also, in a growing child, the molds have to be replaced quite frequently (we were told probably 2 to 3 times a year).
Educators sometimes need the support and direction of medical caregivers. For instance, an FM system (a special type of assistive listening device) can be used by hearing-impaired children in school to amplify the teacher’s voice. The teacher wears a microphone that transmits her voice via radio waves to a receiver that can be attached to the child’s hearing aids, in a speaker mounted in the classroom, or to a personal speaker on the child’s desk. Your child’s healthcare provider should give you detailed information about educational regulations for young people with hearing loss. For more information about education, see Chapter 4 .
The American Academy of Audiology offers information about hearing loss on its consumer website at www.howsyourhearing.org . Links to various websites related to hearing loss in children can be found at www.cdc.gov/ncbddd/hearingloss/links.html . In addition, the Children’s Oncology Group’s survivorship guidelines include an informational resource about hearing loss at www.survivorshipguidelines.org .
Table of Contents
All Guides- 1. Survivorship
- 2. Emotions
- 3. Relationships
- 4. Navigating the System
- 5. Staying Healthy
- 6. Diseases
- 7. Fatigue
- 8. Brain and Nerves
- 9. Hormone-Producing Glands
- 10. Eyes and Ears
- 11. Head and Neck
- 12. Heart and Blood Vessels
- 13. Lungs
- 14. Kidneys, Bladder, and Genitals
- 15. Liver, Stomach, and Intestines
- 16. Immune System
- 17. Muscles and Bones
- 18. Skin, Breasts, and Hair
- 19. Second Cancers
- 20. Homage
- Appendix A. Survivor Sketches
- Appendix B. Resources
- Appendix C. References
- Appendix D. About the Authors
- Appendix E. Childhood Cancer Guides (TM)