Childhood Cancer Survivors
The heart
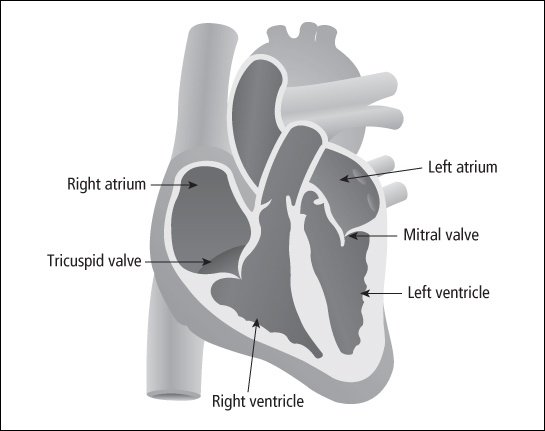
The heart is a four-chambered, muscular organ that pumps blood throughout the body. It is approximately the size of a clenched fist and is located beneath the breastbone (sternum) in the center of the chest cavity. It is a hollow organ with thick walls of cardiac muscle. A double-walled sac called the pericardium surrounds it and helps anchor it in place with connections to the diaphragm and sternum.
The heart has two sides, separated by a thick, muscular wall called the septum. The two upper chambers of the heart are called the right atrium and left atrium. The lower chambers are the left and right ventricles. The atria receive blood coming in from the lungs and the body. They squeeze blood into the ventricles, which then pump it out to the lungs and body.
Valves in the heart prevent blood from flowing backward. The valve between the left atrium and the left ventricle is called the mitral valve, and the valve between the right atrium and right ventricle is called the tricuspid valve. Two other valves are located between the ventricles and the major blood vessels; one leads to the lungs (called the pulmonic valve) and the other to the rest of the body (called the aortic valve). Figure 12-1 shows the anatomy of the heart.
Heart muscle damage from treatment
The muscles in the heart are made up of cells called myocytes. By 6 months of age, an infant heart contains the adult number of myocytes. Further growth of the heart occurs from growth of these existing cells. Chemotherapy drugs called anthracyclines—daunorubicin (Cerubidine ® ), doxorubicin (Adriamycin ® ), epirubicin, and idarubicin—sometimes damage or destroy myocytes. The remaining cells enlarge and stretch to try to compensate for the damage. This can cause thin and stiff ventricular walls, which reduce the heart’s ability to contract effectively.
My two sons both had Wilms tumor. Danny had 175 mg/m 2 (milligrams per square meter of body surface area) of Adriamycin ® at 1 year old and Bobby had 300. They get echocardiograms every 3 years and will switch to a more frequent schedule when they start puberty. They are both doing great and neither has any late effects of any sort.
If the muscle of the heart is weakened, the heart may not pump as well as usual. This is called cardiomyopathy. Some survivors with early stage cardiomyopathy don’t have any symptoms, while others have problems if the heart can no longer keep up with the demands brought on by growth, pregnancy, isometric exercise (e.g., weight lifting, pull-ups, push-ups), or activities of daily life.
Chemotherapy
The number of cells destroyed or damaged is related to the dose of anthracyclines, whether the heart was also irradiated, and other risk factors such as being female and age (children younger than age 2 are at highest risk and younger than age 5 are at high risk). In addition, there are other risk factors that are not yet known or understood.
Anthracyclines can also interfere with the rhythm of the heart and how signals are carried through the heart to make it beat regularly. Children treated with anthracyclines may be at risk for rhythm and conduction problems of the heart that can result in irregular heartbeats, called arrhythmia.
Some protocols incorporate drugs such as dexrazoxane (Zinecard ® ) to see if they will minimize damage from anthracyclines. During the last 3 decades, researchers have learned more about the long-term cardiac effects of anthracyclines, and lower cumulative doses are now being used whenever possible. 1
My daughter was treated for rhabdomyosarcoma in the sinuses at age 9. She had radiation to the tumor (none to her chest) and relatively low doses of anthracyclines. Her echocardiogram at the end of treatment was normal. Since she was not at high risk for cardiac damage, the follow-up clinic did an echo 3 years later and found, to our horror, that her ventricles were very thin and her cardiac function was low (shortening fraction in the 20s). She is now enrolled in a clinical trial evaluating whether enalapril will prevent any further heart damage and improve heart function.
All survivors who were given anthracyclines should be periodically checked for cardiac damage for the rest of their lives. It is not clear what dose of anthracyclines is safe, but certainly higher doses at younger ages are more worrisome than lower doses at older ages. Also, many survivors with changes in the pumping ability of the heart have no symptoms and the changes may not at all interfere with life activities. Consequently, it is important for survivors to know about possible cardiac effects, be checked for them on a regular basis, and discuss any abnormal test results with their healthcare providers.
Anthracyclines are not the only drugs that can damage the heart. Very high doses of cyclophosphamide (Cytoxan ® ) given in preparation for a stem cell transplant may also cause heart damage. The walls of the left ventricle may thicken, leading to heart problems years or decades later. This rare complication may worsen if the child or teen also had radiation to the chest and/or received anthracyclines.
The risk of developing heart problems may be greatest for survivors who had changes in their cardiac function noted on an electrocardiogram (EKG) or echocardiogram during or shortly after the end of therapy. Very long-term research studies are needed to determine who is most at risk.
Radiation
High-dose radiation can cause several late effects to the heart. Children or teens who received high-dose spinal radiation of more than 3000 centigray (cGy), chest radiation (for Hodgkin lymphoma or non-Hodgkin lymphoma), left flank radiation (for Wilms), or radiation directly to the heart are possibly at risk. Modern radiation techniques using lower total doses, hyperfractionation (smaller doses more often), and cardiac shielding (protecting the heart from radiation) are much less likely to cause damage. It is hoped that the use of proton therapy will reduce damage to healthy organs.
Whether the heart sustains injury after radiation treatment depends on several factors, including the following:
-
Total radiation dose
-
Dose of radiation fractions
-
Amount and areas of the heart treated
-
Presence of tumor in or next to the heart
-
Chemotherapy drugs used
Age, weight, blood pressure, family history, smoking, and cholesterol levels do not change the likelihood of developing heart damage, but can magnify its effect later in life in those who have damage.
I had 300 mg/m 2 of Adriamycin ® and 2500 to 2800 cGy of mantle radiation to treat my Hodgkin’s disease. I get echocardiograms periodically, and so far they have been fine. The echo technician always turns the screen around and explains what he’s doing. I appreciate that.
Damage to the heart muscle from high-dose radiation can lead to restrictive cardiomyopathy and arrythmias. Restrictive cardiomyopathy is when the heart muscle becomes stiff and the heart cannot adequately fill with blood. This may lead to problems in the pumping action of the heart. Valves in the heart can also be damaged by radiation (see later section in this chapter about valve damage).
Signs and symptoms
Restrictive cardiomyopathy. Restrictive cardiomyopathy can develop months, years, or decades after treatment for childhood cancer ends. The early signs and symptoms of restrictive cardiomyopathy include the following:
-
Increasing fatigue
-
Decreased ability to exercise
-
Shortness of breath, especially with exercise
-
Feeling full after only a few bites of food
-
Increased difficulties with regular activities of daily life
If you have any of the risk factors for heart damage, these signs and symptoms should prompt you to get a thorough evaluation of your heart. Fatigue alone can be caused by a multitude of things, but if it is getting worse or is accompanied by other symptoms, get it checked out.
Later signs and symptoms of restrictive cardiomyopathy include the following:
-
Swollen lower legs and feet (called edema)
-
Rapid or irregular heartbeat
-
Rapid breathing
-
Difficulty exercising
-
Dizziness
-
Chest pain
Arrhythmia. The electrical pathways that control the heart’s rhythm can be damaged by treatment, which can result in arrhythmia (i.e., abnormally fast, slow, or irregular heartbeat). You may be asymptomatic or may have some of the following symptoms:
-
Palpitations (a feeling that the heart is beating strongly)
-
Rapid heartbeats
-
Skipped beats
-
Dizziness or lightheadedness
-
Fainting
Some healthcare providers (doctors and nurse practitioners) are not aware of the risks for heart problems from your treatment for childhood cancer. If you find this to be the case, get a second opinion from a healthcare provider who is well versed in cardiac late effects associated with cancer treatment.
My radiation-induced cardiac disease was misdiagnosed for years and I almost died. I counsel other survivors to seek out a cardiologist who has seen some irradiated hearts. It wasn’t until I saw a very experienced doctor at a major medical center that my congestive heart failure was correctly diagnosed, although I had seen many cardiologists. It took someone who had seen many, many irradiated hearts to know what to look for.
When I was in a medically oriented graduate program, they taught us this little saying, “When you hear hoofbeats, think horses, not zebras.” That was to warn us to think about the most common things that go wrong with a person, not to think about the exotic or unusual. When someone my age (late 40s) ends up with an inflamed pericardium, viral pericarditis would be the horse. But with a history of mantle radiation, you have to think zebras.
The signs and symptoms for radiation-induced heart damage vary widely. Most damage is caused by higher doses (more than 4000 cGy) and older radiation techniques. Children and teens treated for Hodgkin lymphoma with mantle radiation using modern doses and heart shielding appear to be less likely to develop heart problems, but they still need to be followed over time to see if any long-term late effects develop. Some of the coronary arteries cannot be protected by shielding because of their location. Survivors who were treated in the 1960s and 1970s and those who received high doses of radiation to the chest need to be followed closely to monitor heart function.
Screening and detection
Survivors at risk for late cardiac damage are those who received anthracyclines and/or radiation to the heart (which can occur during radiation to the chest, whole lung, left kidney, and possibly the spine). Even if there are no symptoms, any survivor who received these therapies should have an annual examination to identify risk for cardiac deterioration, to help decide the best medical management, and to guide lifestyle choices. The minimum testing should include:
-
Thorough medical history.
-
Fasting blood levels of cholesterol, HDL, and LDL (only for adults).
-
Physical examination.
-
Chest x-ray.
-
Echocardiogram.
-
12-lead EKG.
-
Cardiac stress test, which may be used in survivors who have abnormalities noted on EKG and echocardiogram or in patients who received intensive treatment that may damage the heart.
My daughter had Wilms tumor many years ago. Our clinic doesn’t have a follow-up program per se, they just see us once a year and take blood and x-rays and ask if she’s having any problems. Since her protocol back then was surgery and high doses of actinomycin D, vincristine, and Adriamycin ® , I asked them last year to do an echocardiogram. They said they only do it if there’s a problem, but I said it would make me feel better if they did it. We went around and around. I finally just put my foot down and said, “I want it.” They did it, it was fine, and now I feel better.
The type of routine cardiac screening for survivors of childhood cancer depends on the treatment received. For cardiomyopathy, an echocardiogram is done (how often is based on a variety of factors). Cardiac magnetic resonance imaging (MRI) provides additional information for survivors diagnosed with cardiomyopathy. Routine screening for survivors who received treatment that could affect the heart must be performed for the rest of their lives.
Intervals between screenings may be longer for those at lesser risk. Ongoing research studies are helping to define the types of evaluations necessary and determine how often they need to be done. See Table 1 at the end of this chapter for more information.
In addition, any survivor at risk for cardiac problems should get a baseline evaluation and systematic follow-up testing when about to undergo increased stress to the heart. Following are examples of activities that stress the heart:
-
Starting an exercise program
-
Being pregnant
-
Getting general anesthesia
-
Taking growth hormone
-
Doing isometric weight lifting (bench presses or squats)
Any changes in the EKG or other cardiac tests require a consultation with a cardiologist experienced in treating survivors of childhood cancer.
I had Adriamycin ® as part of my treatment for osteosarcoma. In my first year of college, I started having severe chest pains that would last from a few seconds to 5 or 6 minutes. Then my chest would ache for a long time afterwards. The pains would frequently wake me up at night. If I got upset it would hurt even more. I went back to my oncologist and he did an EKG and an echocardiogram. He said there was an irregularity, but it was nothing to worry about. I still get the pains once or twice a month.
In the example above, it would be a good idea to find out exactly what the “irregularity” was and to request a referral to an experienced cardiologist for further evaluation. Some survivors report that they have to insist on referrals because they are often young and healthy looking and may see healthcare providers who are not familiar with cardiac late effects from cancer treatment.
My son’s first Wilms tumor stretched from his diaphragm to his bladder. He had 2400 rads (cGy) of left flank radiation that included his spinal cord. When he relapsed, he had more radiation plus lots of cyclophosphamide. They could not shield his left ventricle that time because of the position of the tumor. He started getting pneumonia frequently, had a bad cough, and was really tired all of the time. We were worried so we got a second opinion from an expert in late effects (our hospital did not have a follow-up clinic at the time). She said that kids who had left side Wilms and received radiation do get some radiation to the heart. So taking that into account along with the Adriamycin ® , whole lung radiation, and boost to the para-aortic area, she said he must have follow-up and we have to take seriously that heart damage is a possibility. So he had an echocardiogram and an EKG, and is scheduled for pulmonary function tests.
In the example above, the parents went to an expert and their son is getting appropriate follow-up. Many survivors with heart damage have no symptoms, so it is especially important to get thorough follow-up from a healthcare provider with experience treating survivors of childhood cancer.
Medical management
Routine screening for damage to the heart is usually done by pediatric oncologists or internists. If abnormalities are identified (e.g., pericardial thickening, ventricular wall stiffness), a referral to a cardiologist with experience treating survivors of childhood cancer should be made.
My son was diagnosed with high-risk T-cell ALL (acute lymphoblastic leukemia) in 1996. His white blood cell count was 465,000. He was supposed to get 360 mg of doxorubicin but only received 300. It did some damage to his heart and he was put on enalapril. After his last echo, the cardiologist said his heart was functioning in the normal range. He said he would have to be followed closely when he goes through puberty and the teen growth spurts, due to strain that the heart goes through at that time.
Treatment of cardiomyopathy from anthracyclines or radiation may include ACE inhibitors (such as enalapril) and beta blockers. Cardiac glycosides (such as digoxin) and diuretics, such as furosemide (Lasix ® ), are also used for survivors with congestive heart failure. In some rare cases of severely progressive disease, heart transplantation is considered.
The wall of Clare’s left ventricle has thinned due to Adriamycin ® and her heart function is low normal. She had a dose well below the supposed threshold for heart changes, but they are now finding that some patients are having damage at the lower doses, though not many. No one knows the prognosis, but her doctors are optimistic that it is good. She is enrolled in a double-blind, placebo-controlled, randomized study using enalapril. After 10 months she is doing fine, and her heart function and wall thickness are stable, so we suspect she is really on the drug, but who knows.
Cardiac rehabilitation may also improve heart function and quality of life for survivors with heart damage.
I started cardiac rehab back in the early spring after my last visit with the cardiologist, who had nothing to offer for either my pain or my increasing shortness of breath. I suggested a course of cardiac rehab, but he was very reluctant, saying that it was contraindicated in cases of restrictive cardiomyopathy. I pushed on with this plan with him and my insurance company.
The first sessions were ugly! It was hard to see just how little I could do and how easily I ran out of breath. But in the first two sessions I did learn that if I walked very slowly, I could walk for a very long time without becoming short of breath. Now we are talking a snail’s pace here, but it was comforting to know and helped in my everyday life because I had a lot more energy and could last a lot longer if I just slowed myself down. I also made the first big discovery about my pain. Some of what I had been calling chest pain was really neck, shoulder, and back pain. And with that knowledge I could make some interventions to help with that. So I have started doing some of my old jazz dance relaxation exercises, and that pain has decreased noticeably. Progress is slow but steady.
Lifestyle counseling is necessary for survivors with heart damage. The discussion should emphasize eating a healthy diet, maintaining a normal weight, developing an exercise program, reducing stress, and not smoking cigarettes or using street drugs. Many healthcare providers caution survivors at significant risk for heart problems to limit isometric exercise as it can stress the heart, but they encourage aerobic exercise. Examples of isometric exercises are weight lifting, wrestling, football, and rock climbing.
Some over-the-counter medications include ingredients that can stress the heart; it’s important to read labels and avoid taking medicines that have pseudoephedrine in them. Many illegal drugs (such as cocaine and various forms of amphetamines, including ecstasy and crystal methamphetamine) stress the heart and should not be taken. A rapid rise in blood alcohol levels can cause an irregular heartbeat, so excessive or binge drinking should be avoided. Some prescription drugs can be toxic to the heart. If you have cardiac problems, get a list from your cardiologist of medications to avoid. Pregnant survivors at risk for heart damage from anthracyclines should see an obstetrician who specializes in high-risk pregnancy, as well as a cardiologist.
Preventing heart problems
You cannot prevent the damage already done to the heart from chemotherapy or radiation. However, you can control some things that can lessen your risk of heart damage worsening as you age. To keep your heart as healthy as possible, you can:
-
Not smoke (or quit if you smoke now).
-
Not use drugs that stress the heart such as cocaine, ephedra, diet pills, or sport performance-enhancing drugs.
-
Eat only healthy fats, and make sure they don’t make up more than 30 percent of your calories.
-
Maintain a healthy body weight.
-
Exercise at least 30 minutes every day (but if you have heart problems now, check with your cardiologist before starting an exercise program and minimize isometric exercises).
-
See a cardiologist if you are female, plan to get pregnant, and had anthracyclines and/or radiation to your heart.
Table of Contents
All Guides- 1. Survivorship
- 2. Emotions
- 3. Relationships
- 4. Navigating the System
- 5. Staying Healthy
- 6. Diseases
- 7. Fatigue
- 8. Brain and Nerves
- 9. Hormone-Producing Glands
- 10. Eyes and Ears
- 11. Head and Neck
- 12. Heart and Blood Vessels
- 13. Lungs
- 14. Kidneys, Bladder, and Genitals
- 15. Liver, Stomach, and Intestines
- 16. Immune System
- 17. Muscles and Bones
- 18. Skin, Breasts, and Hair
- 19. Second Cancers
- 20. Homage
- Appendix A. Survivor Sketches
- Appendix B. Resources
- Appendix C. References
- Appendix D. About the Authors
- Appendix E. Childhood Cancer Guides (TM)