Childhood Cancer
Subcutaneous port
Several types of subcutaneous (under the skin) ports are available. The subcutaneous port differs from the external catheter in that it is completely under the skin. A small metal chamber (1.5 inches in diameter) with a rubber top is implanted under the skin of the chest. A catheter threads from the metal chamber (portal) under the skin to a large vein near the collarbone, and then inside the vein to the right atrium of the heart (see Figure 13-2). Whenever the catheter is needed for a blood draw or infusion of drugs or fluid, a needle is inserted by a nurse through the skin and into the rubber top of the portal. Usually a topical numbing agent such as EMLA® is used to make the needle insertion less painful.
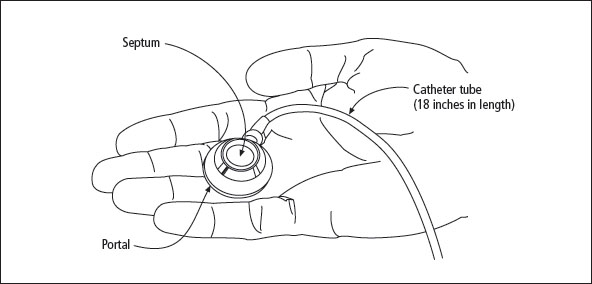
Figure 13-2: Parts of the subcutaneous port
How it’s put in
The subcutaneous port is implanted under general anesthesia; the procedure generally takes less than an hour. The surgeon makes two small incisions: one in the chest where the portal will be placed, and the other near the collarbone where the catheter will enter a vein in the lower part of the neck. First, one end of the catheter is placed in the large blood vessel of the neck and threaded into the right atrium of the heart. The other end of the catheter is tunneled under the skin where it is attached to the portal. Fluid is injected into the portal to ensure the device works properly. The portal is then placed under the skin of the chest and stitched to the underlying muscle. Both incisions are then stitched closed. The only evidence that a catheter has been implanted are two small scars and a bump under the skin where the portal rests.
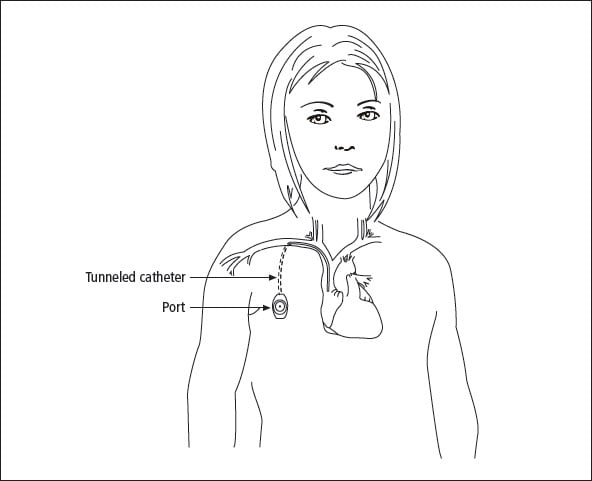
Figure 13-3: Subcutaneous port
Before my child’s surgery to have a port implanted, I saw other children being wheeled into the operating room screaming and trying to climb off the gurney to return to the parents. It broke my heart. When it was Jennifer’s turn, I asked them to give her enough premedication so that she was relaxed and happy to go. I also insisted that I be in the recovery room when she awoke.

How it works
Christine had her port surgery late at night. The resident gave her some premedication, then the chief resident ordered him to give her more. She felt so silly that she looked at me, giggled, and said “Mommy has a nose as long as an elephant’s.” I asked the surgeon if I could be in the recovery room before she awoke, and he said, “Sure.” When I told the nurse that I had permission to go in recovery, she refused. When I persisted, she became angry. I told her that my child was expecting to wake up seeing my face, and I wanted to be there. I suggested that she go in and ask the surgeon to resolve the impasse. When she came out, she let me in the recovery room.
Because the entire subcutaneous port is under the skin, a needle is used to access it. The skin is thoroughly cleansed with antiseptic, and then a special needle is inserted through the skin and the rubber top of the portal. The needle is attached to a short length of tubing that hangs down the front of the chest. A topical anesthetic cream (see Chapter 10, Coping with Procedures) can be applied 1 hour before the needle poke to anesthetize the skin, or ethyl chloride (“freezy spray”) can be sprayed on right before the poke. Subcutaneous ports have a rubber top (septum) that reseals after the needle is removed. It is designed to withstand years of needle insertions, as long as a special “non-coring” needle is used each time. Fluid will leak into the tissues if the wrong needle is used.
If the child is in a part of treatment that requires using the line every day, the nurse will attach the tubing to IV fluids or will close the end off with a sterile cap after flushing the line with saline solution. A transparent dressing will be put over the site where the needle enters the port. The port can remain accessed in this way for up to 7 days. After that time, to avoid the risk of infection, the needle should be removed and the port reaccessed when necessary. If the needle and tubing are to be left in place, it is important to tape them securely to the chest to avoid accidents.
Molly (3 years old) hated tape removal, so we did not secure the IV tubing to her stomach or chest. On one of her many trips to the potty, we accidentally tugged on the tubing and caused a very small tear in the skin around the needle. It became infected. We did home antibiotics on the pump and felt very fortunate that we were able to clear the line with antibiotics. We were glad our doctor was not too quick to remove the line, but it did require 2 weeks off chemotherapy.
If the port is only needed infrequently, the sequence of events is: clean the site, put in the needle, rinse the line with saline, give the drug or draw blood, rinse the line with saline, add heparin to the line, withdraw the needle, and place an adhesive bandage over the site.
Care of the port
The entire port and catheter are under the skin and therefore require no daily care. The skin over the port can be washed just like the rest of the body. Frequent visual inspections are needed to check for swelling, redness, or drainage. Signs of infection include redness, swelling, pain, drainage, or warmth around the port. Fever, chills, tiredness, and dizziness may also indicate that the line has become infected. You should notify the doctor immediately if any of these signs are present or if your child has a fever above 101° F (38.5° C).
My son had a PORT-A-CATH® for 3 years, from age 14 to 17. During that time, he played basketball, football, softball, and threw the shot put in track. His port was placed on his left side just below his armpit. For football, I worked with the trainer and we developed a special pad that went into a pocket I sewed into some T-shirts. That way the port had a little extra padding. We also found shoulder pads that had a sidepiece that covered the area. He never had any problems or soreness from the port.
The subcutaneous port must be accessed and flushed with saline and heparin at least once every 30 days, which might coincide with clinic visits or blood draws. This procedure is done by a nurse or technician. Ports don’t require maintenance by a parent.
Risks
My 3-year-old had a port inserted for a period of about a year and a half. His port survived all kinds of normal kid wear and tear. I remember that kids with external lines were discouraged from swimming, but with a subcutaneous port, there weren’t any restrictions in activity or special precautions, which meant one less thing for us to worry about.
The risks for a subcutaneous port are similar to those for an external catheter: infection, clots, and, rarely, kinks or rupture. If the needle is not properly inserted through the rubber septum, or if the wrong kind of needle is used, fluids can leak into the tissue around the portal.
My son (8 years old) has had a PORT-A-CATH® for 33 months with absolutely no problems. He uses EMLA® to anesthetize it prior to accessing. He hates finger pokes so much that he has his port accessed every time he needs blood drawn.
Infection
We had a few unusual problems in the beginning with the catheter. It was a bit kinked where the catheter went under the collarbone and would not easily draw. This caused more stress than anything in the hospital, because their middle-of-the-night blood draws were always an ordeal for our daughter. They needed to wake her up and try multiple manipulations. Once we were familiar with its idiosyncrasies and were outpatient, we worked it out much better. Then about halfway through treatment, her catheter broke at the kink and travelled into her heart. To make a long story short, it was retrieved by a cardiologist without major surgery, and she got a new one placed, this time with the catheter going down from her neck. It works like a dream.
Most studies show that the infection rate for subcutaneous ports is lower than that of external catheters. If the subcutaneous port does become infected, it is treated the same way an infected external catheter is treated.
Kinks, clots, and ruptures
Katy had two infections in her PORT-A-CATH® during treatment. One occurred when the tape loosened during a blood transfusion. She developed a fever the next day and required 14 days of vancomycin. Eighteen months later, we went in for her monthly chemo, and she became ill in the car on the way home. Her skin became white and clammy, and she felt faint and nauseated. She spiked a 102° temperature, which only lasted for 2 hours. The blood culture both times grew staphylococcus epi.
These events rarely occur with a subcutaneous port. If they do occur, they are treated as described in the external catheter section.
My son had a very bad blood clot in his PORT-A-CATH®. In fact, he had two. He was put on Lovenox® (low molecular weight heparin) for 3 months (twice a day). We went for an ultrasound last week and it showed that the clots are mostly gone now.

When we got to the clinic for weekly chemo, no matter what gravity-defying positions we tried (raising arms, lying down, standing up), our nurse couldn’t get the line to flush. Adrienne’s port was clogged. Luckily, they were able to clear the line with an injection of streptokinase, although it meant entertaining her in the clinic for more than an hour while we waited for it to work. They did tell us that if this didn’t work we’d have to go in overnight for slow infusion of chemo, but the line cleared, and we did chemo outpatient.
Table of Contents
All Guides- Introduction
- 1. Diagnosis
- 2. Bone Sarcomas
- 3. Liver Cancers
- 4. Neuroblastoma
- 5. Retinoblastoma
- 6. Soft Tissue Sarcomas
- 7. Kidney Tumors
- 8. Telling Your Child and Others
- 9. Choosing a Treatment
- 10. Coping with Procedures
- 11. Forming a Partnership with the Medical Team
- 12. Hospitalization
- 13. Venous Catheters
- 14. Surgery
- 15. Chemotherapy
- 16. Common Side Effects of Treatment
- 17. Radiation Therapy
- 18. Stem Cell Transplantation
- 19. Siblings
- 20. Family and Friends
- 21. Communication and Behavior
- 22. School
- 23. Sources of Support
- 24. Nutrition
- 25. Medical and Financial Record-keeping
- 26. End of Treatment and Beyond
- 27. Recurrence
- 28. Death and Bereavement
- Appendix A. Blood Tests and What They Mean
- Appendix B. Resource Organizations
- Appendix C. Books, Websites, and Support Groups

