The Childhood Cancer Blog
The Childhood Cancer Blog

As Rebecca finished treatment for Ewing sarcoma, her cousin, Jacob, was diagnosed with cancer.

Rebecca interned with ALSF in during the summer of 2025, inspired by Jacob's fight and with a desire to help find cures for all children.

One the hard parts of treatment was missing out on everything: college, theater, and her curls.

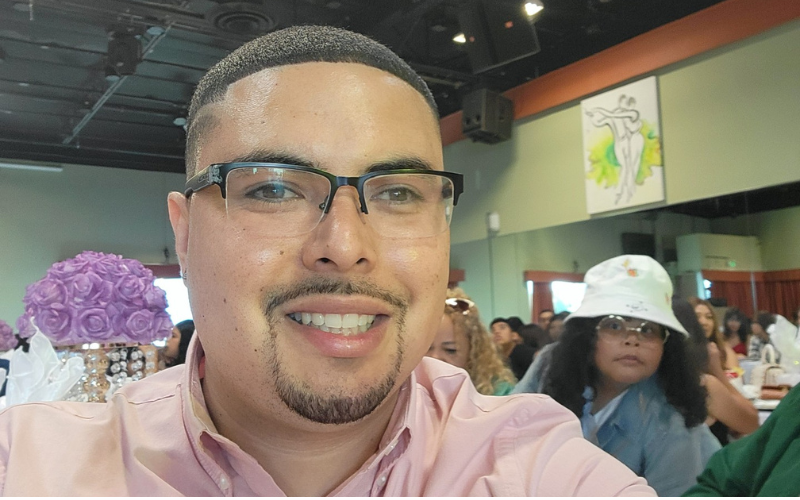
Rebecca with her cousins Lilah and Jacob
When I was emerging from months of difficult cancer treatment, I experienced the most happiness I had in a long time and anticipated a family celebration. However, in the cruelest of twists: my cousin Jacob was diagnosed with cancer.
Jacob was diagnosed with rhabdomyosarcoma and was treated at Lehigh Valley Hospital and Children's Hospital of Philadelphia. We had a “Team Jacob” Facebook page where family and friends could be kept in the loop about his treatment and where we could all spread some... Read More

Sonia was 11 years old when she was diagnosed with Ewing sarcoma. Treatment failed. But then Sonia began a new trial, one funded, in part, by ALSF, for a targeted drug used in combination with chemotherapy.
Sarcoma Awareness Month is every July, and at Alex’s Lemonade Stand Foundation, we’re shining a spotlight on pediatric sarcomas — a group of rare and often aggressive cancers that affect bones and soft tissues in children, adolescents and young adults.
While sarcomas make up just 15% of childhood cancers, their impact is anything but small. Understanding what sarcomas are — and why more research is urgently needed — is an important part of supporting children and families facing these diagnoses.
What is sarcoma?
The origins of the word sarcoma comes from two Greek words... Read More
My name is Chris Ramirez, and I’m a three-time cancer survivor. When I was 17, I was diagnosed with a type of brain cancer called glioblastoma and was given less than two months to live. Today, I’m 33 and healthy.
It all began in 2009 during the second semester of my senior year of high school when I started getting severe headaches. At the time, I was a star baseball player, captain of the team, with college scouts looking at me to go pro. It wasn’t until I had a stroke that my life turned upside down and I received a diagnosis.
I began treatment at UCSF with an amazing... Read More
Pages