The Childhood Cancer Blog
The Childhood Cancer Blog
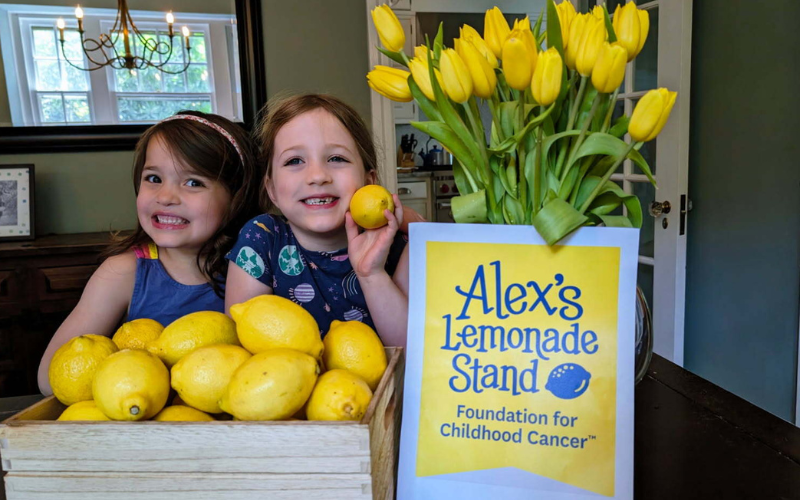
Who could’ve known that some lemons, a home-made stand, and a jar full of money could have formed the foundation of a long-lasting legacy? It’s been 25 years since Alex Scott, the founder of Alex’s Lemonade Stand Foundation (ALSF), held her first lemonade stand, and, ever since, supporters from across the country have found the courage to join the fight by hosting their very own front yard lemonade stands to help fund childhood cancer research.
Whether you’re thinking about joining the movement or have already... Read More

Karen with her son, Tony

Sarah and her son Connor

Kennedy with her family, including kids Karter Rose, Christopher, Kade, and Kylo
The week her daughter, Samantha, was born changed Karen Salerno’s life in ways she never would have imagined. She had imagined going from one child to two children. She had imagined the differences in raising a daughter versus a son. She had thought about how her 2 ½ year old, Tony, would react to being a big brother and sharing his parents' attention. She worried about juggling it all and the early sleepless nights, and long, potentially colicky days.
All normal concerns for a second-time mom. And then, Tony was... Read More

When Lauren graduates, Lauren plans on turning lemons into lemonade by using her unique experiences in a clinical setting to offer the sincerest personal support to her patients.

Maisie is taking classes to become a certified medical assistant and plans to attend nursing school to become a nurse midwife.
Every childhood cancer hero faces unique challenges on the path to finding their cure. That’s why having a dedicated and compassionate medical team can make all the difference. National Nurses Week is celebrated each May in honor of all the devoted healthcare workers whose care and expertise helps their patients.
For childhood cancer heroes Lauren and Maisie, their experiences in the hospital didn’t just give them a future – it determined how they wanted to spend it. After spending some of their most formative years in treatment, here are two heroes who are using their careers to... Read More
Pages